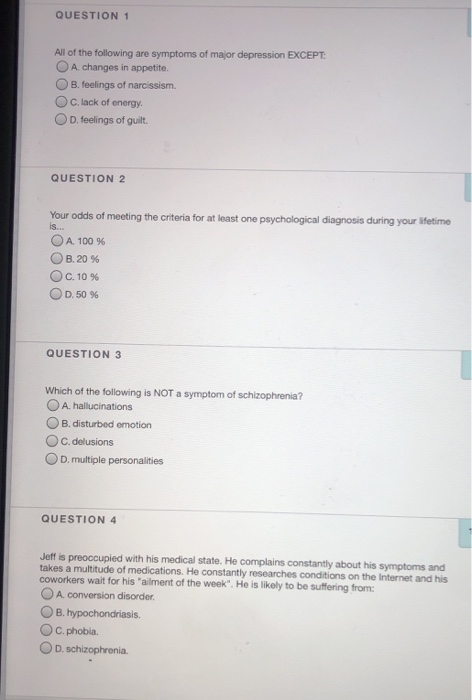
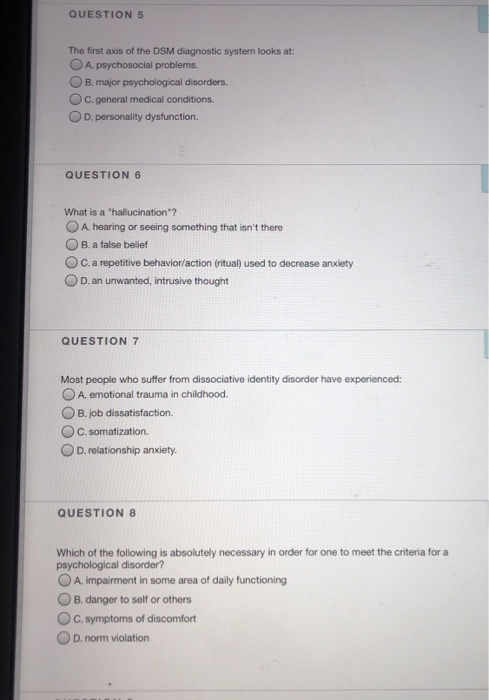
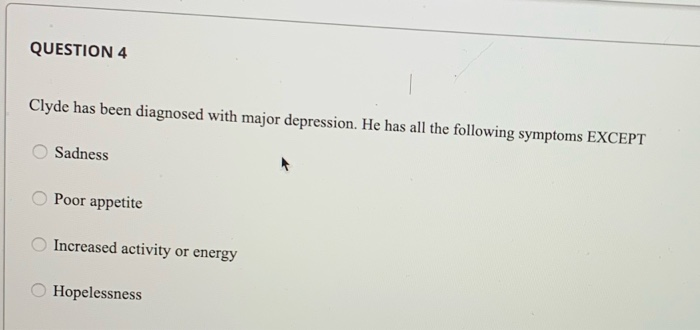
all of the following are symptoms of major depressive disorder except
 Solved: QUESTION 1 All Of The Following Are Symptoms Of Ma... | Chegg.com
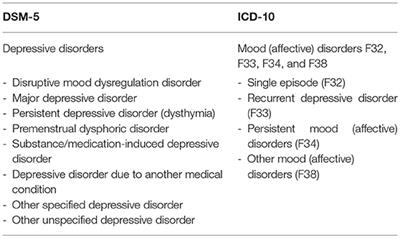
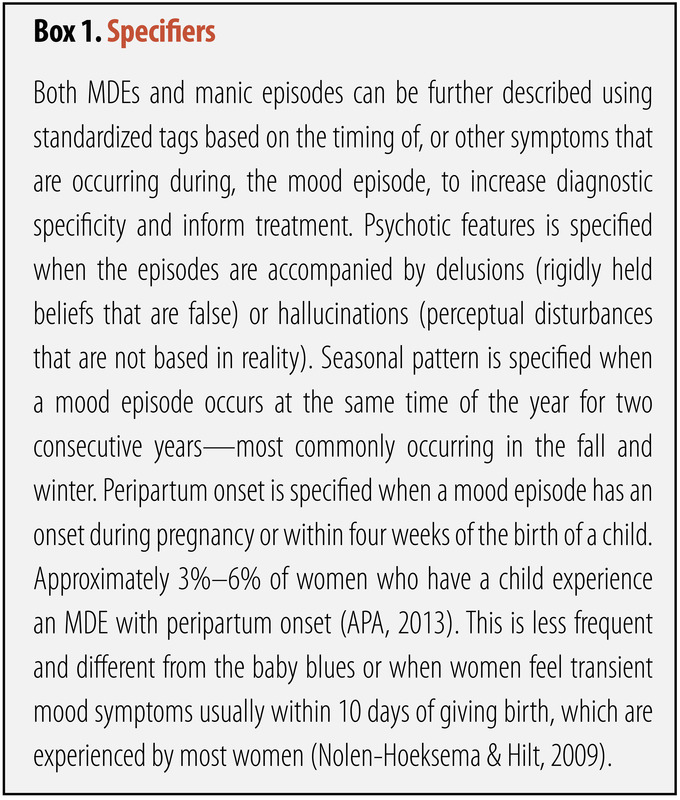
Solved: QUESTION 1 All Of The Following Are Symptoms Of Ma... | Chegg.comMSD Manual Please confirm that you are a health professional Leave this place? The link you selected will take you to a third party website. We do not control or have responsibility for the content of any third party site. OTHER COUNTRIES IN THIS CHAPTER ADDITIONAL CONTENT Try your knowledge More content Depressive disorders By , MD, Carver College of Medicine at University of Iowa The term depression is often used to refer to any of several depressive disorders. Some are classified in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) by specific symptoms: (often called major depression) (distimia)Others are classified by etiology: Depressive disorder due to another medical condition Depressive disorder induced by substances/medicationDepressive disorders occur at any age, but are usually developed at least 20 years. In primary care, up to 30% of patients have depressive symptoms, but Demoralization and pain The term depression is often used to describe the low or discouraging mood that results from disappointments (e.g. financial calamity, natural disaster, serious illness) or losses (e.g., death of a loved one). However, better terms for such moods are demoralization and pain. Negative feelings of demoralization and pain, unlike those of depression, do the following: Happens in waves that tend to be tied to thoughts or reminders of the inciting eventResolve when circumstances or events improve You may be intercalated with periods of positive emotion and humor Are not accompanied by omnipresent feelings of lack of value and self-sufficiency Low mood usually lasts days instead of weeks or months, and suicidal thoughts and prolonged loss of function are much less likely. However, events and stressors that cause demoralization and pain can also precipitate , especially in vulnerable people (e.g. those with past history or family history of major depression). Etiology The exact cause of depressive disorders is unknown, but genetic and environmental factors contribute. The inheritance represents about half of the etiology (less in late depression). Thus, depression is more common among the 1st grade relatives of depressed patients, and the concordance between identical twins is high. In addition, genetic factors probably influence the development of depressive responses to adverse events. Other theories focus on changes in levels of neurotransmitter, including abnormal regulation of neurotransmission (noradrenergic or dopaminergic), glutamatoryrgic and serotonergic (5-hydroxytriciaptamine). Neuroendocrine disregulation can be a factor, with special emphasis on 3 axes: hypothalamic-pituitary-adrenal, hypothalamic-hythyroidal and growth hormone. Psychosocial factors also seem to be involved. Tensions of the larger life, especially separations and losses, tend to precede episodes of major depression; however, such events do not usually cause lasting, severe depression except in people predisposed to a mood disorder. People who have had a major depression episode are at greater risk for later episodes. People who are less resilient and/or who have anxious tendencies can be more likely to develop a depressive disorder. Such people often do not develop social skills to adapt to the pressures of life. Depression can also develop in people with other mental disorders. Women have a higher risk, but no theory explains why. Possible factors include: Increased exposure or increased response to daily stresses Higher levels of oxidase monoamine (the enzyme that degrades neurotransmitters considered important to mood) Endocrine changes that occur with menstruation and menopause In peripartum depression, symptoms develop during pregnancy or within 4 weeks after delivery (); endocrine changes have been involved, but the specific cause is unknown. peripartal depression, In seasonal affective disorder, symptoms develop in a seasonal pattern, typically during autumn or winter; the disorder tends to occur in climates with long or severe winters. Seasonal affective disorder, symptoms or depressive disorders may accompany various physical disorders, including, benign, malignant, , , , , and (see table ). Certain drugs, such as corticosteroids, some beta-blockers, interferon and reserpina, may also result in depressive disorders. The abuse of some recreational drugs (e.g., ) may lead to depression or accompany it. Toxic effects or removal of medications can cause transient depressive symptoms. Some causes of depression and mania symptoms* Type of disorder Depression Mania Conjunct fabric SLE Endocrine Hyperthyroidism Infectious General () Viral AIDS General Influenza St. Louis Neoplastic Disseminated carcinomatosis - Neurological (temporary Wolf) (front left) Complex partial seizures (temporary) Diencephalic tumors Cranial trauma Multiple sclerosis Stroke Nutrition - Other or - Farmacologic Amphotericin B Anticholinesterase Insecticides Beta-blockers (some, for example, propranolol) Cimetidine Corticosteroids Cycloserin Estrogen therapy Indomethacin Interferon Mercury Metildopa Metoclopramide Fenotiazines Reserpine Thallium Vinblastine Vincristine Certain antidepressants Bromocriptine Corticosteroids Levodopa Metilfenidato Sympathetic drugs Mental (except mood disorders) in the initial phase - ♪ Depression usually occurs in these disorders, but no causal relationship has been established. Type of disorder Depression ManiaConective tissueSLEEndocrineHyperthyroidismInfectiousGeneral paresis ()Viral AIDSGeneral paresisInfluenzaSt. Louis encephalitisNeoplasticDisseminated carcinomatosis—Neurologic (temporary wolf) (front left) Complex partial seizures (temporary wolf) Cranial trauma Multiple sclerosisStrokeNutritional— Other insecticides of anfotericin or —Pharmacologica BAnticholinesterasa Beta-blockers (some, for example, propranolol) CimetidineCorticosteroidsCycloserineTherapystrogenIndomethacinInterferonMethyldopaMetochlorpramidePhenothiazinesReserpineThalliumVinblatines Depression usually occurs in these disorders, but no causal relationship has been established. Reference etiology1. : Mechanisms of action and clinical efficacy of NMDA receptor modulators in mood disorders. Neurosci Biobehav Rev 80:555-572, 2017. doi: 10.1016/j.neubiorev.2017.07.002. Symptoms and signs Depression causes cognitive disorders, psychomotors and other types of dysfunction (e.g., poor concentration, fatigue, loss of sexual desire, loss of interest or pleasure in almost all activities that were previously enjoyed, sleep disorders), as well as a depressed mood. People with depressive disorder usually have thoughts of suicide and can try to kill themselves. Other symptoms or mental disorders (e.g., and ) coexist commonly, sometimes complicating diagnosis and treatment. Patients with all forms of depression are more likely to abuse alcohol or other recreational drugs in an attempt to self-treat sleep disorders or anxiety symptoms; however, depression is a less common cause of alcohol consumption disorders and other substance consumption disorders that were once thought. Patients are also more likely to become heavy smokers and to neglect their health, increasing the risk of development or progression of other disorders (e.g. [COPD]). Depression can reduce protective immune responses. Depression increases the risk of cardiovascular disorders, (MIs), and perhaps because in depression, cytokines and factors that increase blood clotting are high and the variability of heart rate is decreased, all potential risk factors for cardiovascular disorders. Greater Depression (universal disorders) Patients may seem miserable, with weeping eyes, dim eyebrows, twisted corners of the mouth, deplomated posture, poor eye contact, lack of facial expression, small body movement and speech changes (e.g., soft voice, lack of prosodium, use of monosylabia words). Appearance can be confused with . In some patients, the depressed mood is so deep that tears dry; they report that they cannot experience habitual emotions and feel that the world has become colorless and lifeless. Nutrition can be severely affected, which requires immediate intervention. Some depressed patients neglect personal hygiene or even their children, other loved ones or pets. For the diagnosis of major depression, ≥ 5 of the following should have been present almost every day during the same period of 2 weeks, and one of them should be depressed mood or loss of interest or pleasure: For the diagnosisDepression of humor most of the dayBest or loss of weight or increased appetiteInsomnia (often persistent sleep-maintenance symptoms) or hypersomniaAgitation or suicide retardation Symptoms usually start insidious during adolescence and may persist for many years or decades. The number of symptoms usually fluctuates above and below the threshold for the major depressive episode. The affected patients may usually be bleak, pessimistic, humorless, passive, lethargic, introverted, hypercritical of oneself and others, and complaining. Patients with PDD are also more likely to have underlying, , or . For the diagnosis of persistent depressive disorder, patients should have had a depressed mood during most of the day for more days than for ≥ 2 years more ≥ 2 of the following: For diagnosisPoor appetite or excess of foodInsomnia or hypersomnia Low energy or fatigue Self-esteem low concentration or difficulty making decisions Pre-destructive feelings Symptoms should be present during most menstrual cycles during the last year. The manifestations are similar to those of but are more severe, causing clinically significant problems and/or marked deterioration of social or occupational functioning. The disorder can begin at any time after the merciarchy; it may worsen as menopause approaches but ceases after menopause. Prevalence is estimated at 2 to 6 per cent of women menstruants at a 12-month interval. For the diagnosis of premenstrual dysphoric disorder, patients should have ≥ 5 symptoms during the week before menstruation. Symptoms should begin to be referred within a few days after the appearance of menses and become minimal or absent in the week after menstruation. Symptoms should include ≥ 1 of the following: For diagnosisChanges of humor marked (e.g., suddenly feel sad or cryful) irritability or anger marked or increased interpersonal conflicts Marked mood depressed, feelings of despair or self-dependant thoughts marked anxiety, tension or feeling of on-edge In addition, inflammation 1 of the following should be present: Less interest in the usual activities Other depressive disordersThe clusters of symptoms with depressive disorder characteristics that do not meet the full criteria for other depressive disorders, but which cause clinically significant or impaired anguish of functioning are classified as another depressive disorder (small or unspecified). Recurrent periods of dysphoria with ≥ 4 other depressive symptoms that last SpecifiersThe major depression and depressive persistent disorder may include one or more specifiers that describe additional manifestations during a depressive episode: Difficult anxiety: Patients feel tension and unusually restless; they have difficulty concentrating because they worry or fear that something terrible may happen, or feel they may lose control of themselves. Anxious discomfort: Mixed Characteristics: Patients also have ≥ 3 manic or hypomanic symptoms (e.g., high mood, grandioseness, greater conversity than usual, flight of ideas, reduced sleep). Patients who have this type of depression are at risk of developing. Mixed characteristics: Melancholic: Patients have lost pleasure in almost all activities or do not respond to pleasant stimuli. They can be depressive and desperate, feel excessive or inappropriate guilty, or have early morning awakening, psychomotor delay marked or agitation, and significant anorexia or weight loss. Melancholic: Atypical: The mood of patients is temporarily shining in response to positive events (e.g., a visit of children). They also have ≥ 2 of the following: excessive reaction to perceived criticism or rejection, feelings of lead paralysis (a heavy or weighted sensation, usually in the extremities), weight gain or increased appetite, and hypersomnia. Atyptic:Psicotic: Patients have delusions and/or hallucinations. Deceptions often involve committing sins or inconceivable crimes, harboring incurable or shameful disorders, or being persecuted. Hallucinations can be auditory (e.g. hearing accusatory or condemnatory voices) or visual. If only the voices are described, it should be taken into account if the voices represent true hallucinations. Psychotic: Catatonic: Patients have severe psychomotor delay, perform excessive activities without purpose and/or withdraw; some patients smile and mimic speech (echolalia) or movement (echopraxia). Catatonic: Beginning of the peripart: The beginning is during pregnancy or in 4 weeks after delivery. Psychotic features may be present; infanticide is often associated with psychotic episodes that involve command hallucinations to kill the baby or delusions that the baby is possessed. Perpartum Active: Reasonable Pattern: Episodes occur at a particular time of the year, most of the time autumn or winter. Seasonal pattern: Diagnosis Clinical Criteria (DSM-5)Full blood count (CBC), electrolytes and thyroid-stimulating hormone (TSH), vitamin B12 and folate levels to rule out physical disorders that may cause depressionDiagnosis of depressive disorders is based on the identification of symptoms and signs and clinical criteria described above. To help differentiate depressive disorders from changes in the ordinary mood, there must be significant discomfort or impairment in the social, occupational or other important areas of operation. Several short questionnaires are available for selection. They help produce some depressive symptoms but cannot be used alone for diagnosis. First-level specific questions help determine whether patients have the symptoms required by DSM-5 criteria for diagnosis of major depression. Gravity is determined by the degree of pain and disability (physical, social, occupational) and by duration of symptoms. A doctor should gently but directly ask patients about any thought and plans to harm themselves or others, any prior threat of or attempts at, and other risk factors. Psychosis and catatony indicate severe depression. Melancholic characteristics indicate severe or moderate depression. Existing physical conditions, and can add to gravity. Differential DiagnosisDepressive disorders should be distinguished from demoralization and pain. Other mental disorders (e.g.) may imitate or hide the diagnosis of depression. Sometimes more than one disorder is present. Higher depression (universal disorder) should be distinguished from . In older patients, depression may manifest as dementia of depression (formerly called pseudodemence), which causes many of the symptoms and signs of psychomotor delay and decrease concentration. However, early dementia can cause depression. In general, when diagnosis is uncertain, treatment of depressive disorder should be treated. Differentiating depressive chronic disorders, such as dystymy, can be difficult, especially because they can coexist and contribute to each other. Physical disorders should also be excluded as a cause of depressive symptoms. It often causes symptoms of depression and is common, especially among older patients. , in particular, can manifest with symptoms that depression micro (e.g., energy loss, lack of expression, lack of movement). A thoroughness is needed to exclude this disorder. Tests No laboratory finding is pathognomonic for depressive disorders. However, laboratory tests are necessary to exclude physical conditions that can cause depression. Tests include full blood count, thyroid-stimulating hormone levels and routine electrolytes, vitamin B12 and folate levels and, in older men, testosterone levels. Evidence for illicit drug use is sometimes appropriate. Treatment SupportPsystemDrugs(See also .)Symptoms may refer spontaneously, especially when they are mild or short-lived. Mild depression can be treated with general support and psychotherapy. Moderate to severe depression is treated with medicines, psychotherapy or therapy as much as electroconvulsant at times. Some patients require a combination of medication. The improvement may not be evident until after 1 to 4 weeks of drug treatment. Depression is likely to be repeated, especially in patients who have had an episode of ≥n 1; therefore, serious cases often require long-term maintenance medication therapy. Most people with depression are treated as outpatients. Patients with significant suicidal ideation, particularly when family support is lacking, require hospitalization, as well as those with psychotic symptoms or physical debilitation. In patients with depressive symptoms often resolve within a few months of stopping the use of substances. Antidepressant treatment is much less likely to be effective as long as the use of substances continues., If a physical disorder or toxicity of drugs could be the cause, the treatment is directed first to the underlying disorder. However, if the diagnosis is in doubt or if the symptoms are disabled or include suicidal ideation or despair, a therapeutic trial with an antidepressant or a state-of-the-art stabilizing medicine can help. Physical Disorder ToxicityIntracial support Until the definitive improvement begins, a doctor may need to see patients weekly or biweekly to provide support and education and to monitor progress. Phone calls can complement office visits. Patients and loved ones may be worried or embarrassed by the idea of having a mental disorder. The doctor may help explain that depression is a serious medical disorder caused by biological alterations and requires specific treatment and that the treatment prognosis is good. Patients and loved ones should be reassured that depression does not reflect a defect of character (e.g. laziness, weakness). Telling patients that the path to recovery usually fluctuates helps them to put feelings of hopelessness in perspective and improves adherence. Encourage patients to gradually increase simple activities (e.g. taking walks, exercising regularly) and social interactions must be balanced by recognizing their desire to avoid activities. The doctor may suggest that patients avoid self-blame and explain that dark thoughts are part of the disorder and will disappear. PsychotherapyThe controlled trials during childbirth have shown that psychotherapy, in particular cognitive behavioral therapy and interpersonal therapy, is effective in patients with major depressive disorder, both to treat acute symptoms and to decrease the likelihood of relapse. Patients with mild depression tend to have better results than those with more severe depression, but the magnitude of improvement is greater in those with more severe depression. Depression TherapyDrug classes and drugs can be used to treat depression: (RSS) (5-HT2 blockers) (MAOIs) can be guided by the previous response to a specific antidepressant. Otherwise, ISRS are often the initial medicines of choice. Although different ISRS are equally effective for typical cases, certain properties of drugs make them more or less appropriate for certain patients (see table). Electroconvulsive therapy (CT)Electroconvulsive therapy is often treated with STD if drugs are ineffective: Serious suicidal depressionDepression with agitation or psychomotor retardationDepression during pregnancy Patients who have stopped eating may need treatment to prevent death. ECT is particularly effective for psychotic depression. The response to treatments from 6 to 10 STDs is usually dramatic and can be saved. The relapse after the STD is common, and drug therapy is often maintained after the STD is stopped. Phototherapy Phototherapy is best known for its effects on seasonal depression, but it seems to be equally effective for non-seasonal depression. Treatment can be provided at home with 2500 to 10,000 lux at a distance of 30 to 60 cm for 30 to 60 minutes/day (later with a less intense light source). In patients who sleep late at night and get up late in the morning, phototherapy is more effective in the morning, sometimes complemented by 5 to 10 minutes of exposure between 3 PM and 7 PM. For patients who sleep and get up early, phototherapy is more effective between 3 PM and 7 PM. Other therapies Sometimes psychostimulants are used (e.g. dextroamphetamine, methylphenidate), often with antidepressants. Several controlled trials support their use in depressive disorders (). Psychostimulants Medicinal herbs are used by some patients. can be effective for mild depression, although data are contradictory. San Juan's herb can interact with other antidepressants and other medications. Some placebo-controlled studies of omega-3 supplementation, used as an increase or as monotherapy, have suggested that eicosapentaenoic acid 1 to 2 g once a day has useful antidepressant effects. Herbs Medicinal nerve stimulation involves intermittently stimulating the vague nerve through an implanted pulse generator. It may be useful for refractory depression to other treatments, but usually takes 3 to 6 months to be effective. Vagus Nervous Stimulation The use of repetitive transcranial magnetic stimulation (rTMS) for acute treatment of major depressive disorder has substantial support for controlled trials. Low frequency rTMS can be applied to the right dorsolateral prefrontal cortex (DLPC), and rTMS can be applied to the left DLPC. The most common side effects are headaches and scalp discomforts; both occur more often when high frequency is used instead of low frequency rTMS. Repetitive transcranial magnetic stimulation (rTMS) Deep brain stimulation directed to subgenital cingulate or the previous ventral internal capsule/ventral estre has had promising results in uncontrolled case series (). Controlled trials are underway. Deep Brain Stimulation Support groups (e.g., the Bipolar Depression and Support Alliance []) can help patients by providing a forum to share their common experiences and feelings. Support groups Restoration References1. : The effectiveness of psychostimulants in major depressive episodes: A systematic review and meta-analysis. J Clin Pscyhopharmacol 37 (4):412-418, 2017. doi: 10.1097/JCP.0000000000723.2. : Deep cerebral stimulation of the anterior ventral extremity of the internal capsule for treatment-resistant depression: A randomized clinical trial. JAMA Psychiatry 73 (5):456–64, 2016. doi: 10.1001/jamapsychiatry.2016.0152. Key points Depression is a common disorder that involves depressed mood and/or almost complete loss of interest or pleasure in previously enjoyed activities; somatic (e.g., weight change, sleep disturbance) and cognitive manifestations (e.g., difficulty concentrating) are common. Depression can significantly impair the ability to function at work and interact socially; the risk of suicide is significant. Sometimes depressive symptoms are caused by physical disorders (e.g., thyroid or adrenal gland disorders, benign or malignant brain tumors, strokes, AIDS, Parkinson's disease, multiple sclerosis) or the use of certain drugs (e.g., corticosteroids, some beta blockers, interferon, some recreational drugs). The diagnosis is based on clinical criteria; physical disorders must be discarded by clinical evaluation and selected tests (e.g. CBC; electrolyte, TSH, B12 and folate levels). Treatment involves psychotherapy and usually drugs; ISRS are usually first processed, and if they are ineffective, other drugs that affect serotonin and/or norepinephrine can be judged. Was this page helpful? Also of interest SOCIAL MEDIA MSD and MSD ManualsMerck & Co., Inc., Kenilworth, NJ, USA (known as MSD outside the US and Canada) is a global health leader who works to help the world be well. Since the development of new therapies that treat and prevent diseases to help people in need, we are committed to improving health and well-being around the world. The Manual was first published as the Merck Manual in 1899 as a community service. The legacy of this great resource continues while the MSD Manual outside North America. Learn more about our commitment to this site meets the information:
Solved: QUESTION 1 All Of The Following Are Symptoms Of Ma... | Chegg.com
Solved: QUESTION 5 Which Of The Following Disorders Charac... | Chegg.com
SOLVED:Common symptoms of major depressive disord…

Quiz & Worksheet - Characteristics of Major Depression | Study.com

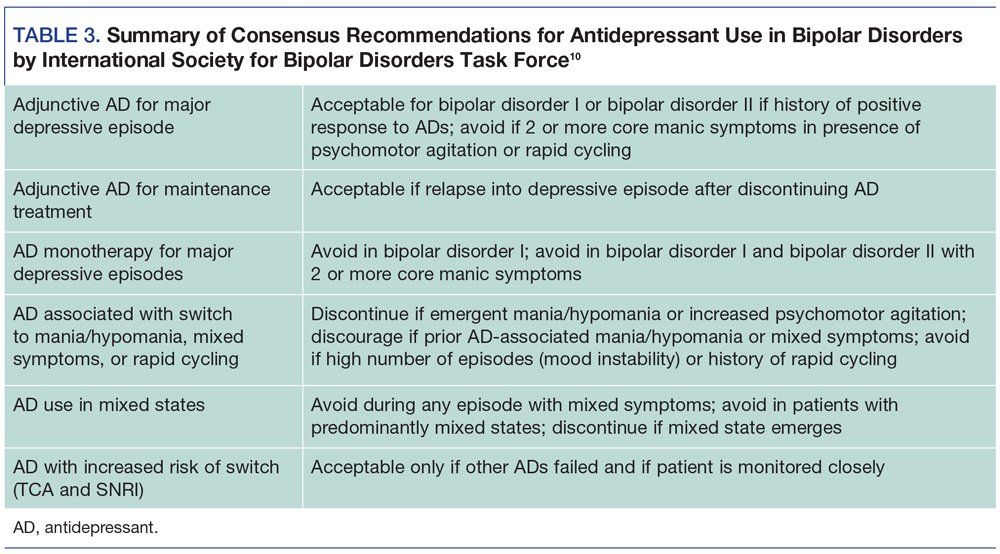
Major Depressive Disorder with Mixed Features - A Review
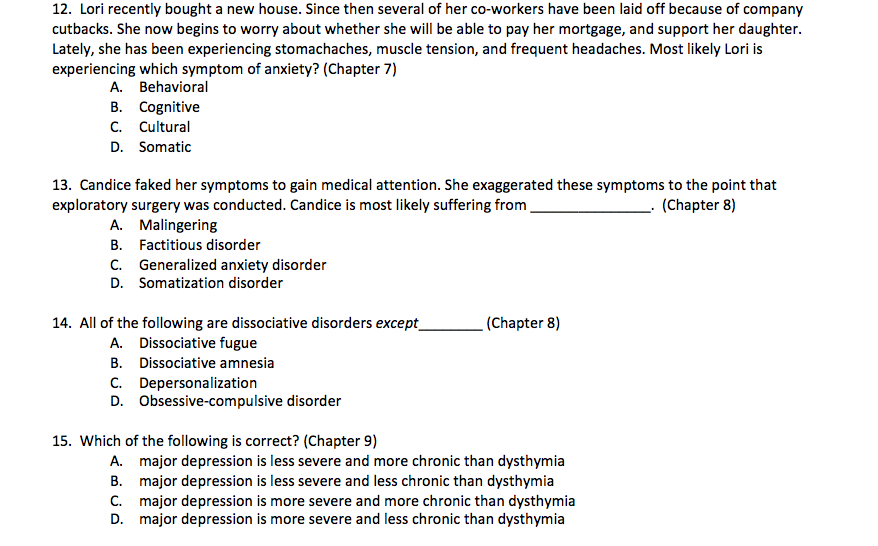
Solved: 12. Lori Recently Bought A New House. Since Then S... | Chegg.com
DEPRESSION Pre-test Questions 1. Which of the following antidepressants is a good first-line choice for this patient? a. Amitrip
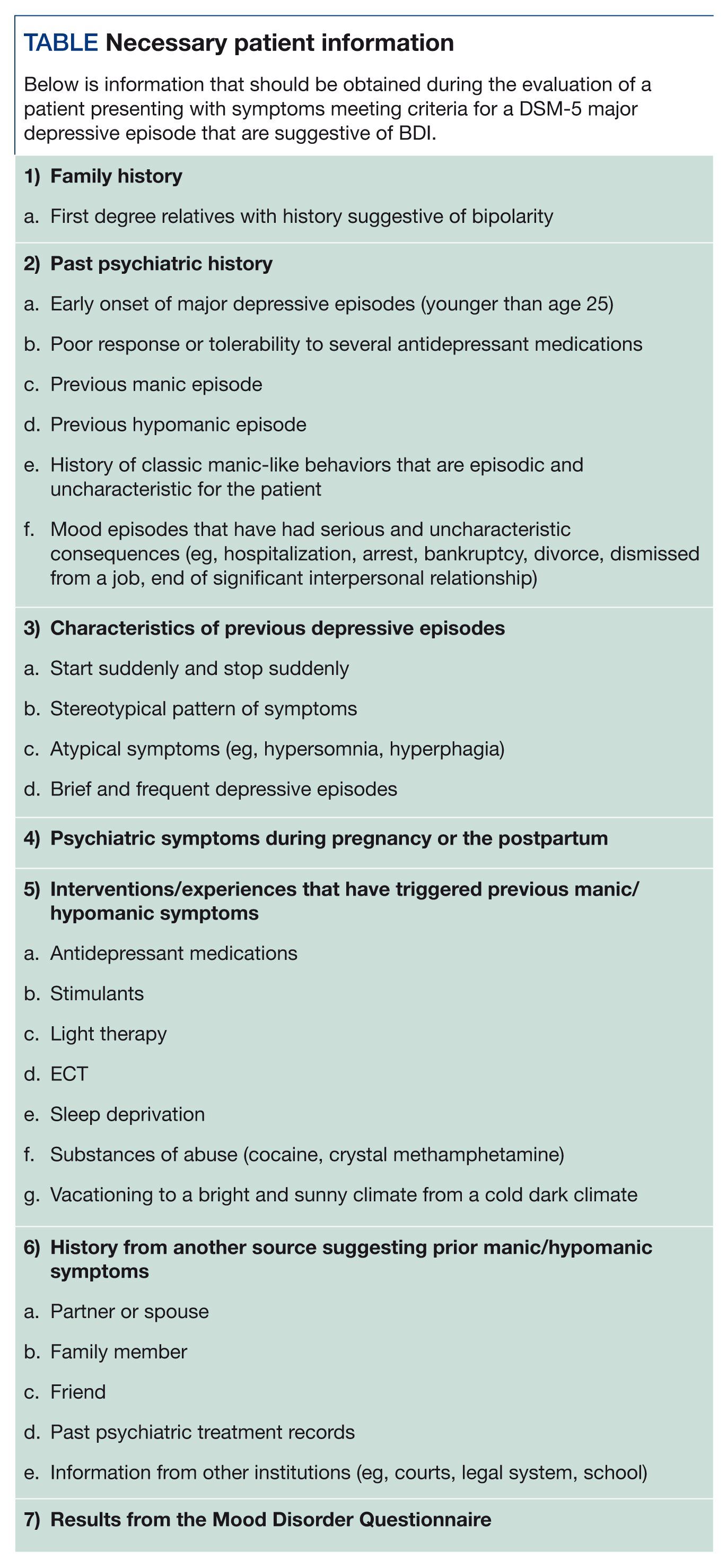
Major Depressive Episode: Is It Bipolar I or Unipolar Depression?
:max_bytes(150000):strip_icc()/1066910-top-depression-symptoms-5ae724e38023b90036653091.png)
Clinical Depression: Signs, Symptoms, and Sub-Types

Major Depressive Disorder: Symptoms, Causes, and Treatment
Major Depressive Disorder With Mixed Features: Recognition and Management
Frontiers | Child and Adolescent Depression: A Review of Theories, Evaluation Instruments, Prevention Programs, and Treatments | Psychology
/maybe-its-not-depression-2330495_final-6ca813926d564fcebd4becf475ba831e.png)
13 Possible Reasons Why You're Tired All the Time
/common-types-of-depression-1067313_V3-c0654a8dc19049a086684d391318514f.png)
7 Most Common Types of Depression

Review of dysthymia and persistent depressive disorder: history, correlates, and clinical implications - The Lancet Psychiatry

Cognitive function following a major depressive episode: a systematic review and meta-analysis - The Lancet Psychiatry

Effect of a stepped-care intervention delivered by lay health workers on major depressive disorder among primary care patients in Nigeria (STEPCARE): a cluster-randomised controlled trial - The Lancet Global Health

Symptoms of Major Depressive Disorder Scale: Performance of a Novel Patient-Reported Symptom Measure - ScienceDirect
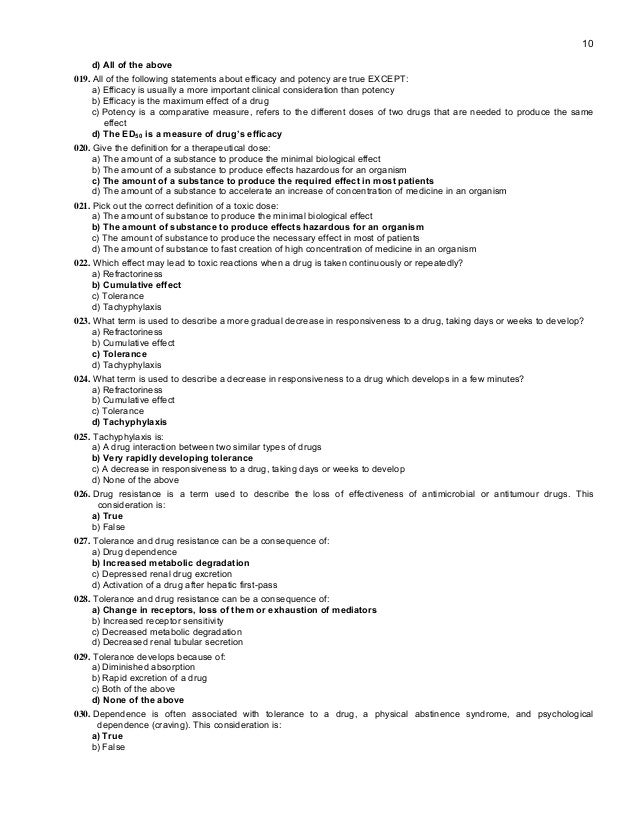
MCQ Pharmacology
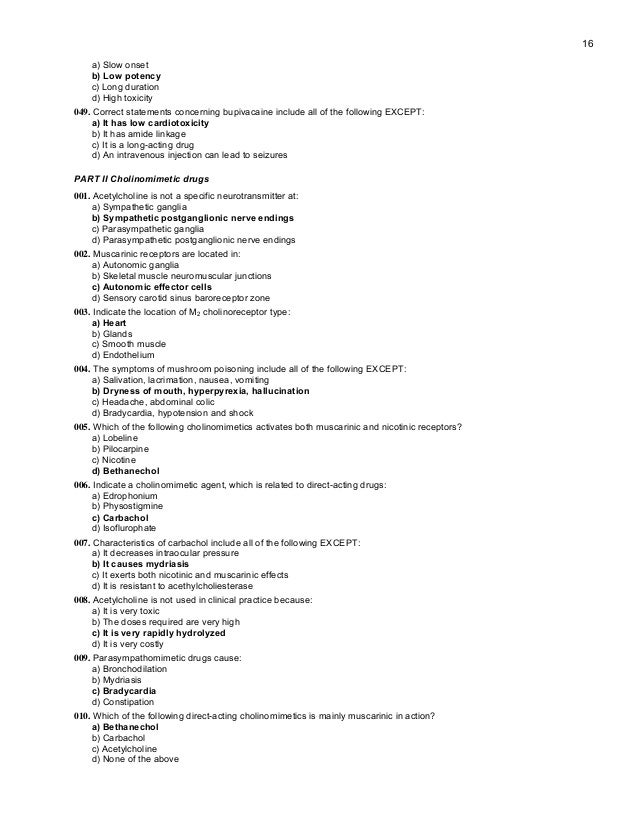
MCQ Pharmacology

Major Depressive Disorder: Symptoms, Causes, and Treatment

Combined prevention for substance use, depression, and anxiety in adolescence: a cluster-randomised controlled trial of a digital online intervention - The Lancet Digital Health

What is Major Depression? The Signs, Symptoms & Treatment
Treatment-Resistant Bipolar Disorder
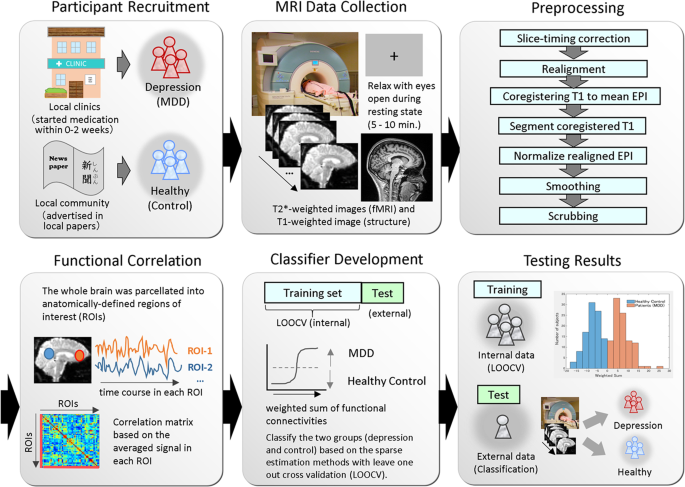
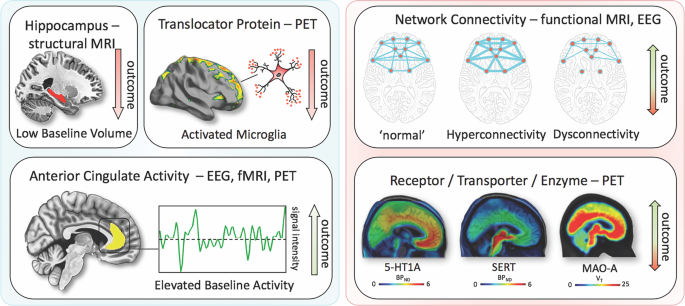
Primary functional brain connections associated with melancholic major depressive disorder and modulation by antidepressants | Scientific Reports
Mental Health - Our World in Data
Mood Disorders | Noba
Treatment of Patients With Major Depressive Disorder
SEALD Endpoint Review Template v5

Types of Depression: The 10 Most Common Depressive Disorders
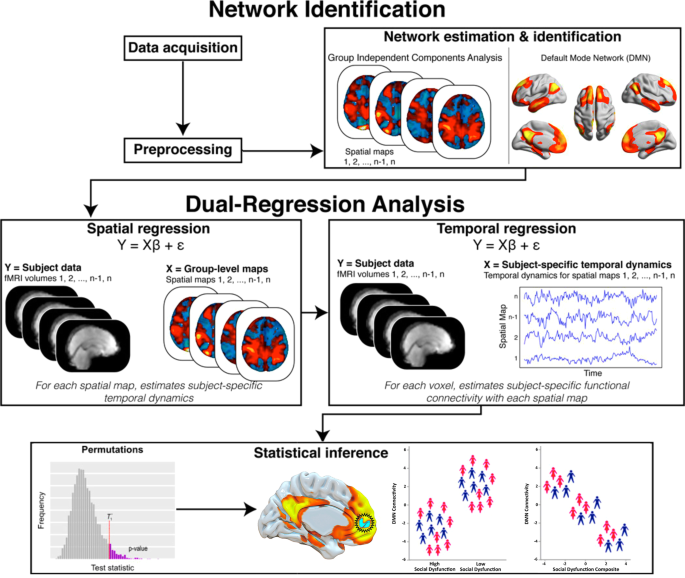
Default Mode Network Connectivity and Social Dysfunction in Major Depressive Disorder | Scientific Reports
Major Depressive Disorder With Mixed Features: Recognition and Management

Treatment of Childhood and Adolescent Depression - American Family Physician
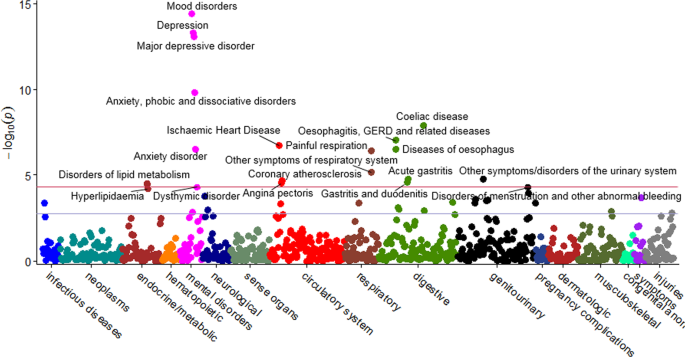
Association between major depressive disorder and multiple disease outcomes: a phenome-wide Mendelian randomisation study in the UK Biobank | Molecular Psychiatry

Depression | ACP Hospitalist

Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study - The Lancet Psychiatry
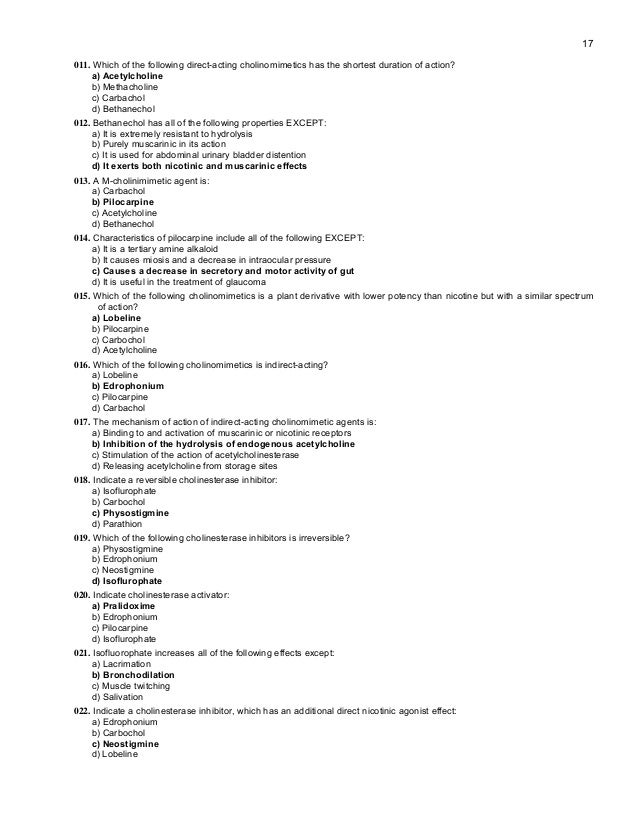
MCQ Pharmacology
Prognosis and improved outcomes in major depression: a review | Translational Psychiatry

Treatment of Childhood and Adolescent Depression - American Family Physician
/symptoms-of-mania-380311_final-237f247e10ae42508e8ca3410453ad81.png)
Symptoms of Mania in Bipolar Disorder
Posting Komentar untuk "all of the following are symptoms of major depressive disorder except"